Mitigate your facility’s risk for an outbreak of Legionnaire’s disease

By Dave Bodenschatz
With nearly 7,500 people contracting Legionnaire’s disease in 2017 – a five-fold increase since 2000 according to the Centers for Disease Control and Prevention – healthcare organizations are assessing the safeguards in place to minimize the risk the acquired disease poses to their patients and staff. However, the disease’s bacteria can exist in any facility that has domestic water systems, a cooling tower, pool, hot tub, or fountain.

This illustration depicts a 3D computer-generated image of a group of Legionella pneumophila bacteria. © CDC
Legionnaire’s disease is caused by the Legionella pneumophilia (Lp) bacteria, which occur naturally and exist in most water systems. The bacteria grow and thrive in stagnant water at a temperature between 77°F and 108°F but can multiply in temperatures between 68°F and 122°F. Infection is generally acquired by inhaling steam or mist from contaminated water from such sources as hot tubs, showers, aerated faucets, fountains, cooling towers, and stagnant domestic water piping that are not properly cleaned and disinfected. People over age 50, transplant patients, those who are immune-suppressed, have chronic lung disease, or a history of smoking are more prone to contracting the disease. Thus, patients in a healthcare setting can be at greater risk.
Several organizations including the CDC and ASHRAE have published standards and guidelines on assessing and minimizing Legionella risk and how to mitigate the bacteria when discovered in domestic water systems. Following are several key strategies based on those standards and guidelines.
Domestic Hot Water Systems
System survey
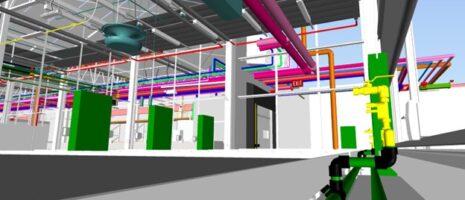
Since Legionella thrives and grows in stagnant and tepid water, it is recommended that a survey be performed on any existing domestic water system. This survey should include a domestic water system diagram.
The survey will review the domestic system for sparsely used fixtures, un-circulated hot water supply piping and possible dead legs – a length of pipe that water doesn’t move through, like a hot water pipe that was capped when the faucet it ran to was moved (creating plumbing with no flow and an increased risk of bacteria growth). Once the current system is analyzed, a plan of correction should be enacted to address the observed issues.
Domestic hot water temperature control
The temperature of water affects the life cycle of the Lp bacteria. Sources vary slightly on exact temperatures, but the following are generally accepted ranges:
Below 68° F: Lp survive but are dormant
68° F to 122° F: Lp growth range
131° F: Lp die within 5 to 6 hours
140° F: Lp die within 32 minutes
151° F: Lp die within 2 minutes
158° F: Disinfection level – instantaneous kill

A CDC microbiologist pours water samples from a building experiencing a Legionnaire’s outbreak into a filtration system to test for Legionella. © CDC
Historically, most plumbing codes and jurisdictions recommended domestic hot water systems be stored at 140° F to kill the Lp. These systems often used a central mixing station to mix the water down to an acceptable range of 110° to 120° F. Water would then be circulated through the building in this range. (Note that this temperature is in the prime Lp growth range.) Today, however, most international, state, and local plumbing codes are being revised to require domestic hot water systems to produce, store, and circulate the water at 140° F. This will require a mixing valve at each fixture to reduce scald risks.
Systems should be circulated at ≥140° F as close as possible to the point of use to reduce the chance of dead legs and reduce the time for water to flow through the fixture. A plan also should be in place to periodically and randomly test “high risk” fixtures for Legionella contamination.
Some codes are considering requiring the system to produce, store, and circulate water at 160° F to promote continuous disinfection. While this may help disinfect the system, it causes other concerns:
A. Fixtures that do not have mixing valves risk scalding or burns to the user. Common fixtures include commercial kitchen wash sinks, dishwashers, and janitor sinks.
B. At locations that include a mixing valve, failure of that valve could again expose users to scalding and burns.
C. Additional energy consumption is needed to maintain hotter water.
D. Additional insulation is required on the system piping to minimize heat loss and increase safety.
Additional suggestions for domestic water systems include:
- Use of instantaneous water heaters where possible to minimize storage of water
- Recirculating hot water and minimizing branch piping lengths to fixtures
- Minimizing the length between thermostatic mixing valves and the fixture outlet
- Exercising fixtures regularly to flush with fresh water
- Adding “dump valves” at the end of runs for domestic cold water systems
- Monitoring all domestic water temperatures to identify unacceptable ranges
- Eliminating dead legs
- Removing aerators on fixtures used by patients
- Reducing or eliminating electronic faucets in high risk locations. (Some sources indicate such faucets have a greater risk of Legionella growth than manual faucets.)
- Cleaning and disinfecting plumbing fixtures
Adding a copper-ion exchange system on the incoming water also may reduce Legionella in the system. Copper-silver ionization releases positively-charged copper and silver ions into the water, which form electrostatic bonds with negatively-charged bacteria cell walls. This bond is thought to disrupt bacterial cell walls and lead to cell death.
If Legionella is detected, the following mitigation strategies can be taken:
- Hot water flushing of the domestic water system. Superheat the water system in the affected area to 160° F. This requires careful coordination with nursing staff and maintenance to plan and communicate which portions of the system will be superheated so that scalding doesn’t occur.
- Hyperchlorination of the system. This also requires careful coordination with nursing staff and maintenance to reduce risks to patients.
Cooling Towers

Cooling towers – often a part of air conditioning systems of large buildings – are a common source of Legionella bacteria and need to be properly maintained to prevent Legionnaire’s disease. © CDC
Any building system that has exposed stagnate water and operates within 68° F to 122° F can promote the growth of Legionella. These systems include pools, hot tubs, and fountains, but cooling towers have the highest associated risk.
Legionella bacteria can grow on the wet surfaces and in the basins of cooling towers, which generally operate in the prime growth range of 68° F to 100° F. The bacteria can become airborne by the fan that circulates air through the tower. The risk can be minimized by ensuring:
- Water has little opportunity to remain stagnate in the basins
- Basins have positive slope to the outlet
- Chemical treatment that includes disinfection as well as corrosion protection
- Chemical treatment feed system is functioning properly
- Regular testing of the water
Conclusion
Healthcare and other types of facilities can significantly reduce their Legionella risk by ensuring their domestic water systems follow the recommendations above and are in accordance with the established guidelines, standards, and codes in force within their jurisdiction.
Regular monitoring and documentation by facilities staff also should be standard procedure, with corrective action taken when needed.
Proper water system design and management will help ensure the health and well-being of patients and staff and help turn the tide of the growing incidence of Legionnaire’s disease nationwide.
If your building needs a Legionella water managements program or remediation services, the CDC suggests working with a Legionella consultant. To help choose the right consultant for your situation, read the CDC’s list of considerations. For information on IMEG’s design experience for minimizing Legionella risk, contact the authors.
Standards, Guidelines, and References
The following organizations have published standards, guidelines and documents on assessing and minimizing Legionella risk and how to mitigate the bacteria when discovered in domestic water systems:
- ASHRAE Guideline12: Guidelines on Reducing the Risk of Legionella
- ASHRAE Standard 188: Risk Management for Building Water Systems
- VHA Directive 2008-10: Prevention of Legionella Disease
- Drinking Water Advisory Communication Toolbox(CDC, U.S. Department of Health and Human Services)
- Developing a Water Management Program to Reduce Legionella Growth & Spread in Buildings (CDC, U.S. Department of Health and Human Services)
- Centers for Disease Control and Prevention
- Legionella.org